Page 18 - Škrgat, Sabina, ed. 2022. Severe Asthma - Basic and Clinical Views. Koper: University of Primorska Press. Severe Asthma Forum, 1
P. 18
management due to inherent biological ther-
apeutic implications8,11,13.
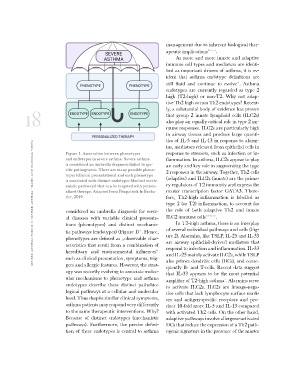
severe asthma forum 1: severe asthma - basic and clinical views Figure 1. Association between phenotypes
and endotypes in severe asthma. Severe asthma As more and more innate and adaptive
is considered an umbrella diagnosis linked to spe- immune cell types and mediators are identi-
cific pathogenesis. There are many possible pheno- fied as important drivers of asthma, it is ev-
types (clinical presentations) and each phenotype ident that asthma endotype definitions are
is associated with distinct endotypes (distinct mech- still fluid and continue to evolve13. Asthma
anistic pathways) that can be targeted with person- endotypes are currently regarded as type 2
alized therapy. Adapted from Fitzpatrick & Bacha- high (T2-high) or non-T2. Why not adap-
rier, 2019. tive Th2 high or non Th2 endotypes? Recent-
ly, a substantial body of evidence has proven
considered an umbrella diagnosis for sever- that group 2 innate lymphoid cells (ILC2s)
al diseases with variable clinical presenta- also play an equally critical role in type 2 im-
tions (phenotypes) and distinct mechanis- mune responses. ILC2s are particularly high
tic pathways (endotypes) (Figure 1)13. Hence, in airway tissues and produce large quanti-
phenotypes are defined as „observable char- ties of IL-5 and IL-13 in response to alarm-
acteristics that result from a combination of ins, mediators released from epithelial cells in
hereditary and environmental influences“ response to stressors, such as infection or in-
such as clinical presentation, symptoms, trig- flammation. In asthma, ILC2s appear to play
gers and allergic features. However, the strat- an early and key role in augmenting the type
egy was recently evolving to associate molec- 2 responses in the airway. Together, Th2 cells
ular mechanisms to phenotype and asthma (adaptive) and ILC2s (innate) are the prima-
endotypes describe these distinct pathobio- ry regulators of T2 immunity and express the
logical pathways at a cellular and molecular master transcription factor GATA3. There-
level. Thus despite similar clinical symptoms, fore, Th2-high inflammation is labelled as
asthma patients may respond very differently type 2 (or T2) inflammation, to account for
to the same therapeutic interventions. Why? the role of both adaptive Th2 and innate
Because of distinct endotypes (mechanistic ILC2 immune cells5,7,11,13.
pathways). Furthermore, the precise defini-
tion of these endotypes is central to asthma In T2-high asthma, there is an interplay
of several individual pathways and cells (Fig-
ure 2). Alarmins, like TSLP, IL-25 and IL-33
are airway epithelial-derived mediators that
respond to infection and inflammation. IL-33
and IL-25 mainly activate ILC2s, while TSLP
also primes dendritic cells (DCs), and conse-
quently B- and T-cells. Recent data suggest
that IL-33 appears to be the most potential
amplifier of T2-high asthma1. Alarmins serve
to activate ILC2s. ILC2s are lineage-nega-
tive cells that lack lymphocyte surface mark-
ers and antigen-specific receptors and pro-
duce 10-fold more IL-5 and IL-13 compared
with activated Th2 cells. On the other hand,
adaptive pathways involve allergens-activated
DCs that induce the expression of a Th2 path-
ogenic signature in the presence of the master
apeutic implications8,11,13.
severe asthma forum 1: severe asthma - basic and clinical views Figure 1. Association between phenotypes
and endotypes in severe asthma. Severe asthma As more and more innate and adaptive
is considered an umbrella diagnosis linked to spe- immune cell types and mediators are identi-
cific pathogenesis. There are many possible pheno- fied as important drivers of asthma, it is ev-
types (clinical presentations) and each phenotype ident that asthma endotype definitions are
is associated with distinct endotypes (distinct mech- still fluid and continue to evolve13. Asthma
anistic pathways) that can be targeted with person- endotypes are currently regarded as type 2
alized therapy. Adapted from Fitzpatrick & Bacha- high (T2-high) or non-T2. Why not adap-
rier, 2019. tive Th2 high or non Th2 endotypes? Recent-
ly, a substantial body of evidence has proven
considered an umbrella diagnosis for sever- that group 2 innate lymphoid cells (ILC2s)
al diseases with variable clinical presenta- also play an equally critical role in type 2 im-
tions (phenotypes) and distinct mechanis- mune responses. ILC2s are particularly high
tic pathways (endotypes) (Figure 1)13. Hence, in airway tissues and produce large quanti-
phenotypes are defined as „observable char- ties of IL-5 and IL-13 in response to alarm-
acteristics that result from a combination of ins, mediators released from epithelial cells in
hereditary and environmental influences“ response to stressors, such as infection or in-
such as clinical presentation, symptoms, trig- flammation. In asthma, ILC2s appear to play
gers and allergic features. However, the strat- an early and key role in augmenting the type
egy was recently evolving to associate molec- 2 responses in the airway. Together, Th2 cells
ular mechanisms to phenotype and asthma (adaptive) and ILC2s (innate) are the prima-
endotypes describe these distinct pathobio- ry regulators of T2 immunity and express the
logical pathways at a cellular and molecular master transcription factor GATA3. There-
level. Thus despite similar clinical symptoms, fore, Th2-high inflammation is labelled as
asthma patients may respond very differently type 2 (or T2) inflammation, to account for
to the same therapeutic interventions. Why? the role of both adaptive Th2 and innate
Because of distinct endotypes (mechanistic ILC2 immune cells5,7,11,13.
pathways). Furthermore, the precise defini-
tion of these endotypes is central to asthma In T2-high asthma, there is an interplay
of several individual pathways and cells (Fig-
ure 2). Alarmins, like TSLP, IL-25 and IL-33
are airway epithelial-derived mediators that
respond to infection and inflammation. IL-33
and IL-25 mainly activate ILC2s, while TSLP
also primes dendritic cells (DCs), and conse-
quently B- and T-cells. Recent data suggest
that IL-33 appears to be the most potential
amplifier of T2-high asthma1. Alarmins serve
to activate ILC2s. ILC2s are lineage-nega-
tive cells that lack lymphocyte surface mark-
ers and antigen-specific receptors and pro-
duce 10-fold more IL-5 and IL-13 compared
with activated Th2 cells. On the other hand,
adaptive pathways involve allergens-activated
DCs that induce the expression of a Th2 path-
ogenic signature in the presence of the master